Endoscopy
Gastroscopy
Gastroscopy is a test to look inside the gullet (oesophagus), the stomach and the first part of the gut (small intestine) known as the duodenum.
What is a gastroscopy?
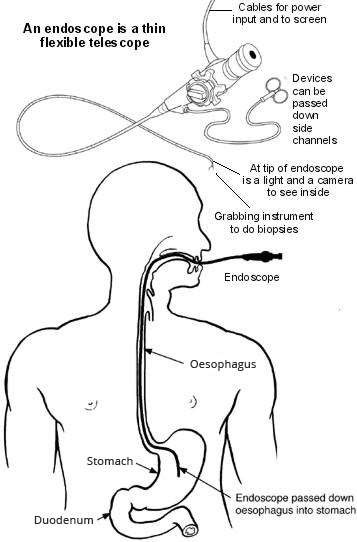
A gastroscopy is a test where a doctor looks into the upper part of your gut (the upper gastrointestinal tract).
The upper gut consists of the gullet (oesophagus), the stomach and the first part of the gut (small intestine) known as the duodenum. The doctor uses an endoscope to look inside your gut. Therefore, the test is sometimes called endoscopy.
An endoscope is a thin, flexible telescope. It is about as thick as a little finger. The endoscope is passed through the mouth, into the oesophagus and down towards the stomach and duodenum.
The tip of the endoscope contains a light and a tiny video camera so the doctor can see inside your gut.
The endoscope also has a side channel down which various instruments can pass. These can be manipulated by the doctor. For example, the doctor may take a small sample (biopsy) from the inside lining of the stomach by using a thin 'grabbing' instrument which is passed down a side channel.
What happens during a gastroscopy?
Gastroscopy is usually done as an outpatient 'day case'. It is a routine test which is commonly done. The doctor may numb the back of your throat by spraying on some local anaesthetic, or give you an anaesthetic lozenge to suck. You may be given a sedative to help you to relax. This is usually given by an injection into a vein in the back of your hand. The sedative can make you drowsy but it does not put you to sleep completely. It is not a general anaesthetic.
You lie on your side on a couch. You are asked to put a plastic mouth guard between your teeth. This protects your teeth and stops you biting the endoscope. The doctor will then ask you to swallow the first section of the endoscope. Modern endoscopes are quite thin but some people may find this difficult. The doctor then gently pushes it further down your gullet (oesophagus) and into your stomach and the first part of your gut (small intestine) known as your duodenum. The video camera at the tip of the endoscope sends pictures to a screen. The doctor watches the screen for abnormalities of the oesophagus, stomach and duodenum. Air is passed down a channel in the endoscope into the stomach to make the stomach lining easier to see. This may cause you to feel full and want to belch.
The doctor may take one or more small samples (biopsies) of parts of the inside lining of the gut - depending on why the test is done and what they see. This is painless. The biopsy samples are sent to the laboratory for testing and to look at under the microscope. The endoscope is then gently pulled out.
A gastroscopy usually takes about 10 minutes. However, you should allow at least two hours for the whole appointment. This is to prepare, give time for the sedative to work (if you have one), for the gastroscopy itself and to recover. A gastroscopy may be quite uncomfortable but it does not usually hurt.
Who has a gastroscopy?
A gastroscopy may be advised if you have symptoms such as:
Repeated (recurring) indigestion.
Recurring heartburn.
Pains in the upper tummy (abdomen).
Repeatedly being sick (vomiting).
Difficulty swallowing.
Other symptoms thought to be coming from the upper gut.
The sort of conditions which can be confirmed (or ruled out) include:
Inflammation of the gullet (oesophagus), called oesophagitis. The doctor will see areas of redness on the lining of the oesophagus.
Stomach ulcer and duodenal ulcer. An ulcer looks like a small, red crater on the inside lining of the stomach or on the first part of the gut (small intestine) known as the duodenum.
Inflammation of the duodenum (duodenitis) and inflammation of the stomach (gastritis).
Stomach and oesophageal cancer.
Various other rare conditions.
What preparation do I need to do?
You should receive instructions from the hospital department before your test. The sort of instructions given commonly include:
You should not eat for 4-6 hours before the test. The stomach needs to be empty. (Small sips of water may be allowed up to two hours before the test.)
If you have a sedative you will need somebody to accompany you home.
Advice about medication which may need to be stopped before the test.
What can I expect after a gastroscopy?
Most people are ready to go home after resting for half an hour or so.
If you have had a sedative - you may take a bit longer to be ready to go home. The sedative will normally make you feel quite pleasant and relaxed. However, you should not drive, operate machinery or drink alcohol for 24 hours after having the sedative. You will need somebody to accompany you home and to stay with you for 24 hours until the effects have fully worn off. Most people are able to resume normal activities after 24 hours.
The doctor writes a report and sends it to the doctor who requested the gastroscopy. The result from any sample (biopsy) may take a few days, which can delay the report being sent. The doctor may also tell you what he/she saw before you leave. However, if you have had a sedative you may not remember afterwards what you were told. Therefore, you may wish to have a relative or close friend with you who may be able to remember what was said.
Is gastroscopy reliable?
Gastroscopy is a good test for seeing abnormalities in the upper gut. However, it is not foolproof. For example, gastroscopy may not detect a small number of cases of early ulcers or early cancer. Sometimes a repeat gastroscopy may be advised if symptoms persist or become worse, even if a previous gastroscopy was reported as normal.
Are there any side-effects or complications from having a gastroscopy?
Most gastroscopies are done without any problem. Some people have a mildly sore throat for a day or so afterwards. You may feel tired or sleepy for several hours if you have a sedative. There is a slightly increased risk of developing a chest infection or pneumonia following a gastroscopy.
Occasionally, the endoscope causes some damage to the gut. This may cause bleeding, infection and (rarely) a hole (perforation). If any of the following occur within 48 hours after a gastroscopy, consult a doctor immediately:
Tummy (abdominal) pain. (In particular, if it becomes gradually worse, and is different from or more intense than any 'usual' indigestion pains or heartburn that you may have.)
Raised temperature (fever).
Difficulty breathing.
Bringing up (vomiting) blood.
A small number of people have a heart attack or stroke during, or soon after, a gastroscopy. These tend to be older people who are already in poor health. These serious complications are rare in most people who are otherwise reasonably healthy.
Rarely, some people have an allergic reaction to the sedative.
Colonoscopy
A colonoscopy is a test to assess your colon (large intestine).
What is a colonoscopy?
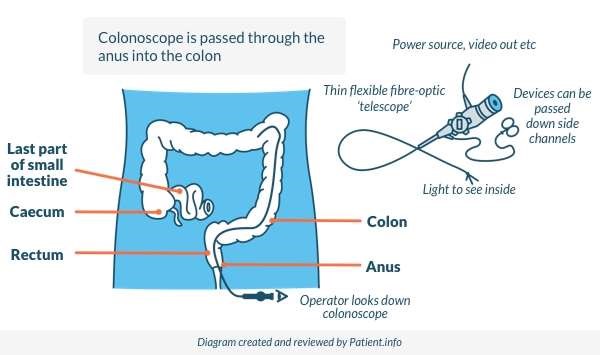
A colonoscopy is a test where a doctor looks into your colon. The colon is sometimes called the large intestine or large bowel. The colon is the part of the gut which comes after the small intestine. The last part of the colon leads into the rectum where stools (faeces) are stored before being passed out from the back passage (anus).
A colonoscope is a thin, flexible telescope. It is about as thick as a little finger. It is passed through the anus and into the colon. It can be pushed all the way round the colon as far as the caecum (where the small and large intestine meet). Another test called sigmoidoscopy looks at the rectum and the lower part of the colon. See the separate leaflet called Sigmoidoscopy for more details.
The colonoscope contains fibre-optic channels which allow light to shine down so the doctor can see inside your colon.
The colonoscope also has a side channel down which devices can pass. These can be manipulated by the doctor. For example, the doctor may take a small sample (biopsy) from the inside lining of the colon by using a thin 'grabbing' instrument which is passed down a side channel.
Who has a colonoscopy?
A colonoscopy may be advised if you have symptoms such as:
Bleeding from the back passage (anus).
Pains in the lower tummy (abdomen).
Persistent diarrhoea.
Other symptoms thought to be coming from the colon.
The sort of conditions which can be confirmed include:
Ulcerative colitis (which causes inflammation of the colon).
Crohn's disease (which also causes inflammation of the colon).
Pouches which form in the lining of the colon (diverticula).
Bowel (colonic) polyps.
Bowel (colorectal) cancer.
Various other conditions may also be detected. Also, a colonoscopy is often normal. However, a normal result may help to rule out certain possible causes of your symptoms.
What happens during a colonoscopy?
Colonoscopy is usually done as an outpatient or day case. It is a routine test which is commonly done. You will usually be given a sedative to help you to relax. This is usually given by an injection into a vein in the back of your hand. The sedative can make you drowsy but it does not put you to sleep. It is not a general anaesthetic.
You lie on your side on a couch. The doctor will gently push the end of the colonoscope into your back passage (anus) and up into the colon. The doctor can look down the colonoscope and inspect the lining of the colon. Also, modern colonoscopes transmit pictures through a camera attachment on to a TV monitor for the doctor to look at.
Air is passed down a channel in the colonoscope into the colon to make the inside lining easier to see. This may cause you to feel as if you want to go to the toilet (although there will be no stools (faeces) to pass). The air may also make you feel bloated, cause some mild 'wind pains', and may cause you to pass wind. This is normal and there is no need to be embarrassed, as the doctor will expect this to happen.
The doctor may take small samples (biopsies) of some parts of the inside lining of the colon - depending on why the test is done. This is painless. The biopsy samples are sent to the laboratory for testing and to be looked at under the microscope. Also, it is possible to remove polyps, which may be found, with an instrument attached to a colonoscope. (Polyps are small lumps of tissue which hang from the inside lining of the colon.) At the end of the procedure the colonoscope is gently pulled out.
A colonoscopy usually takes about 20-30 minutes. However, you should allow at least two hours for the whole appointment to prepare, give time for the sedative to work, for the colonoscopy itself and to recover. A colonoscopy does not usually hurt but it can be a little uncomfortable, particularly when the colonoscope is first passed into the anus.
A newer type of colonoscopy called a virtual colonoscopy is available. It is sometimes known as computerised tomography (CT) colonography or CT colonoscopy. It may be suggested as appropriate for you to have if:
You have had a conventional colonoscopy and your doctor was not able to visualise the entire large bowel.
There are technical reasons why it is difficult to do a colonoscopy.
This type of colonoscopy is performed using a CT scan to take an image of the bowel. A thin tube is put into the back passage to put air into the bowel to help produce clear images. The CT scan then produces images of the large bowel.
What preparation do I need to do?
You should receive instructions from the hospital department before your test. The sort of instructions given include:
The colon needs to be empty so that the doctor can obtain a clear view. You will be instructed on how to take a special diet for a few days before the test. You will also be given some laxatives to take.
You will need somebody to accompany you home, as you will be drowsy with the sedative.
What can I expect after a colonoscopy?
Most people are ready to go home after resting for half an hour or so. You may need to stay a bit longer for observation if you have had any small lumps of tissue (polyps) removed.
If you have had a sedative - you may take a bit longer to be ready to go home. The sedative will normally make you feel quite pleasant and relaxed. However, you should not drive, operate machinery, drink alcohol, take important decisions or sign documents for 24 hours after having the sedative. You will need somebody to accompany you home and to stay with you for 24 hours until the effects have fully worn off. Most people are able to resume normal activities after 24 hours.
The doctor writes a report and sends it to the doctor who requested the colonoscopy. The result from any sample (biopsy) may take a few days, which can delay the report being sent.
The doctor may also tell you what he/she saw before you leave. However, if you have had a sedative, you may not remember afterwards what you were told. Therefore, you may wish to have a relative or close friend with you who may be able to remember what was said.
Are there any side-effects or complications from having a colonoscopy?
Most colonoscopies are done without any problem. The sedative may cause you to feel tired or sleepy for several hours afterwards. You may pass a small amount of blood from your back passage (anus) if a biopsy was taken or if a small lump of tissue (polyp) was removed. You may also have leakage of liquid accompanied by gas for up to 24 hours after taking the last dose of laxatives. You should arrange your work/social activities following a colonoscopy with this in mind.
Occasionally, the colonoscope may cause damage to the colon. This may cause bleeding, infection and (rarely) a hole (perforation). If any of the following occur within 48 hours after a colonoscopy, consult a doctor immediately:
Tummy (abdominal) pain. (In particular if it becomes gradually worse and is different or more intense to any 'usual' pains that you may have.)
Raised temperature (fever).
Passing a lot of blood from your anus.
 A gastroscopy is a test where a doctor looks into the upper part of your gut (the upper gastrointestinal tract).
The upper gut consists of the gullet (oesophagus), the stomach and the first part of the gut (small intestine) known as the duodenum. The doctor uses an endoscope to look inside your gut. Therefore, the test is sometimes called endoscopy.
An endoscope is a thin, flexible telescope. It is about as thick as a little finger. The endoscope is passed through the mouth, into the oesophagus and down towards the stomach and duodenum.
The tip of the endoscope contains a light and a tiny video camera so the doctor can see inside your gut.
The endoscope also has a side channel down which various instruments can pass. These can be manipulated by the doctor. For example, the doctor may take a small sample (biopsy) from the inside lining of the stomach by using a thin 'grabbing' instrument which is passed down a side channel.
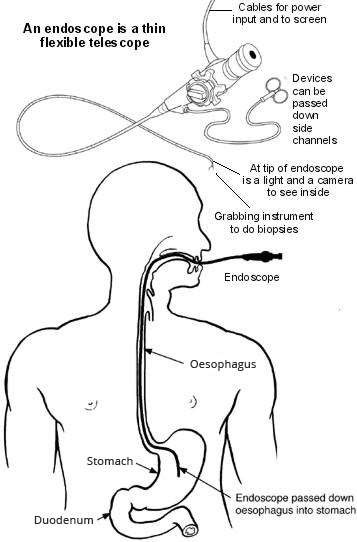
A gastroscopy is a test where a doctor looks into the upper part of your gut (the upper gastrointestinal tract).
The upper gut consists of the gullet (oesophagus), the stomach and the first part of the gut (small intestine) known as the duodenum. The doctor uses an endoscope to look inside your gut. Therefore, the test is sometimes called endoscopy.
An endoscope is a thin, flexible telescope. It is about as thick as a little finger. The endoscope is passed through the mouth, into the oesophagus and down towards the stomach and duodenum.
The tip of the endoscope contains a light and a tiny video camera so the doctor can see inside your gut.
The endoscope also has a side channel down which various instruments can pass. These can be manipulated by the doctor. For example, the doctor may take a small sample (biopsy) from the inside lining of the stomach by using a thin 'grabbing' instrument which is passed down a side channel.
 A colonoscopy is a test where a doctor looks into your colon. The colon is sometimes called the large intestine or large bowel. The colon is the part of the gut which comes after the small intestine. The last part of the colon leads into the rectum where stools (faeces) are stored before being passed out from the back passage (anus).
A colonoscope is a thin, flexible telescope. It is about as thick as a little finger. It is passed through the anus and into the colon. It can be pushed all the way round the colon as far as the caecum (where the small and large intestine meet). Another test called sigmoidoscopy looks at the rectum and the lower part of the colon. See the separate leaflet called Sigmoidoscopy for more details.
The colonoscope contains fibre-optic channels which allow light to shine down so the doctor can see inside your colon.
The colonoscope also has a side channel down which devices can pass. These can be manipulated by the doctor. For example, the doctor may take a small sample (biopsy) from the inside lining of the colon by using a thin 'grabbing' instrument which is passed down a side channel.
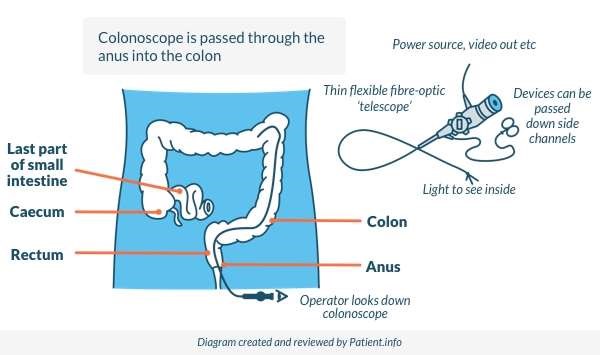
A colonoscopy is a test where a doctor looks into your colon. The colon is sometimes called the large intestine or large bowel. The colon is the part of the gut which comes after the small intestine. The last part of the colon leads into the rectum where stools (faeces) are stored before being passed out from the back passage (anus).
A colonoscope is a thin, flexible telescope. It is about as thick as a little finger. It is passed through the anus and into the colon. It can be pushed all the way round the colon as far as the caecum (where the small and large intestine meet). Another test called sigmoidoscopy looks at the rectum and the lower part of the colon. See the separate leaflet called Sigmoidoscopy for more details.
The colonoscope contains fibre-optic channels which allow light to shine down so the doctor can see inside your colon.
The colonoscope also has a side channel down which devices can pass. These can be manipulated by the doctor. For example, the doctor may take a small sample (biopsy) from the inside lining of the colon by using a thin 'grabbing' instrument which is passed down a side channel.
